
Would you like to have more moments of pure, focused thinking where everything just pours out and flows? Well, there is a way: it’s called the cross-crawl.
Essentially this is a form of cross-lateral body movements- where you use opposite sides of the body to work together (ex: crawling, walking, swimming). This strengthens the bridge between the right and left hemispheres of your brain, allowing for electrical impulses and information to pass freely. In turn, this not only improves physical coordination but thinking-based activities such as reading and focusing.
By doing these movements you are:
-
Building your core strength
-
Releasing stress and tension
-
Enhancing whole-brain thinking
-
Calming your mind
-
Energizing your body
You need reliable, easy, and effective strategies to not only manage stress, but reliably get to peak performance. You need to be able to turn it on when you need to turn it on.
Therefore, do the cross-crawl.

You may have noticed that at any given moment your pain levels can fluctuate based on many different variables, including the weather, how much sleep you got the night before, and whether or not you are having a stressful day. But you may not have given much thought to the role that bacteria might be playing in how you feel.
You have hundreds of different types of bacteria living inside the gut that make up what is referred to as the microbiome, and like a fingerprint, each person’s microbiome is a bit unique but swayed by factors like diet, the environment, and lifestyle habits. Research has shown that the composition of the gut bacteria in healthy people often differs from those with certain diseases, including obesity, heart disease, inflammatory bowel disease, diabetes, autoimmune disorders, and even depression.
As we start to learn more about how our microbiome affects our overall health, we are also starting to see evidence that it can also play a role in how much we hurt.
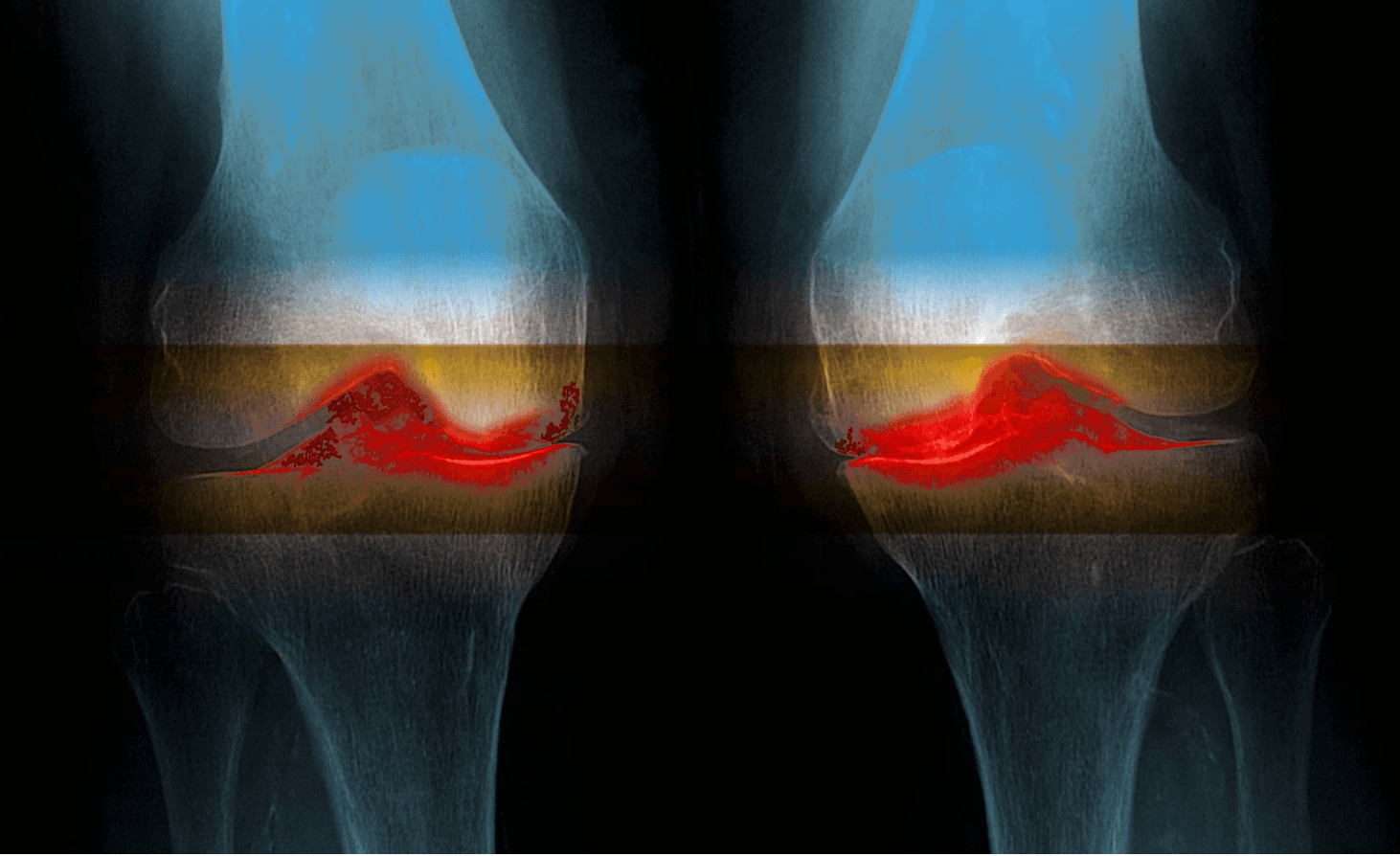
Consider a recent study published by researchers from the University of Rochester that looked at the effects of the microbiome on joint pain and swelling in mice. In comparing the gut bacteria of mice that had been plumped up on an unhealthy diet with mice kept on a healthy diet, they found that the obese mice’s gut bacteria was not only different than that of their slimmer counterparts, it also included inflammation-causing strains. These gut changes coincided with signs of inflammation throughout their bodies, including their joints. The researchers also found that when both sets of mice experienced cartilage damage to their knees, the obese mice with the inflammation-causing gut bacteria experienced a rapid deterioration of their joints compared to the other mice.
In a short amount of time, these unfortunate mice developed advanced osteoarthritis of their knees. When the researchers treated the obese mice with a prebiotic (a food source for growing healthy bacteria in the gut), they were able to prevent the inflammation and arthritic deterioration in their knee joints, without changing their body composition.
This is very interesting research, but despite this and other evidence suggesting that the microbiome can directly impact the amount of inflammation, arthritis, and ultimately the amount of pain that we experience, it is still unclear how to take advantage of this information to treat pain in our everyday lives. Unfortunately, in humans we have not found that simply adding a prebiotic to our diet will make all of the pain and swelling magically disappear. There may be a number of reasons for that, including the wide variation in microbiomes from person to person, and the unique environments that we each live in.
But, just because we don’t know exactly which foods might help improve gut health doesn’t mean we can’t give it try. I’ve personally made it a point to increase my intake of both prebiotics and probiotics (live, beneficial bacteria). Prebiotics can be found in fiber-rich fruits and vegetables, and you can get probiotics in foods like yogurt, kefir, kombucha, kimchi, and sauerkraut, or via supplements. As always, make sure to talk to your doctor before making any big changes or starting a supplement.
BY PETER ABACI, MD
Board-certified anesthesiologist and pain specialist
FEBRUARY 11, 2019
About the author:
Peter Abaci, MD, is one of the world’s leading experts on pain and integrative medicine and serves as the co-founder and Medical Director for the Bay Area Pain & Wellness Center. He is a dedicated healer, author, and radio celebrity. To learn more about Dr. Abaci, visit his website.

Nerve pain, whether it is from a surgical procedure or a nerve injury, the pain is difficult to treat. The patient will usually rely on pain medications, such as antidepressants and nerve blocks. However, there is a longer-lasting method that provides significant relief with side effects.
In a study done by the American Academy of Pain Medicine, 15 neuropathic pain patients with 22 pain syndromes were treated with cross-linked hyaluronic acid injections. Before the treatment , the average pain score was 7.5 out of 10. After the treatment , the score was reduced to a 1.5 out of 10 , with the average duration relief lasting 7.7 months .
Cross-linked HA is an FDA-approved commercially available cosmetic agent, such as Juvederm and Restylane. However, native HA naturally occurs throughout the extracellular matrix (ECM) of the skin in connective, epithelial, and neural tissues. While the native, non-cross-linked form of HA is a liquid and metabolized in a day, the molecular cross-linking of the HA binds its individual polymeric chains and forms a viscoelastic hydrogel, which accounts for its longevity.
In another case, a patient, whose had right hand pain from an operation, was treated with an injection of Restylane. At 4 months , the patient had reported that his right-hand pain remained 75% to 85% improved with no reactions or side effects . The patient described his improvement in pain as ‘dramatic’.
Cross-linked hyaluronic acid is a great treatment method because it augments and sustains many times over the restorative and healing process of the body including:
-
Anti-inflammatory response
-
Inhibition of scar formation
-
Entry into the healing and restoration phase

Regenerative therapy is a relatively new, yet groundbreaking discovery in medicine. With regenerative therapy, we can perform a minimally invasive surgery with longer-lasting results . We can see this especially in the cases of tendinopathy and osteoarthritis .
Case #1: Advanced Tendinopathic Disease
For example, in the case of a lesion in the tendinopathic tissue, doctors performed a tenotomy , which included clearing out the tendinopathic tissue so that the natural healing process would begin, and then to stimulate it with regenerative therapy. The lesion was permeated with platelet rich plasma (PRP) that was taken from the patient. After the operation, a rehabilitation protocol was initiated to ensure the best results. Within four weeks post-op , the patient reported a 60% reduction in pain , and at ten weeks, the patient was able to run with little discomfort.
Case #2: Lateral Osteoarthritis of the Knee
Mesenchymal stem cell (MSC) therapy has gained recognition as a potential treatment for generalized osteoarthritis of the knee. This patient had left knee pain and was treated with oral anti-inflammatories with some benefit. She had also received corticosteroid injections which provided three weeks of symptom improvement, but then pain returned to baseline. Her doctors decided that she needed to be treated with a single injection of bone marrow concentrate and then an intra-articular injection of PRP one month later.
Six months later, the patient’s reported knee injury and Osteoarthritis Outcome Score has improved by a factor of three times the minimal clinically significant difference. One year following the initial treatment, she remains satisfied and has significantly lower pain than before .
In conclusion, regenerative therapy provides the potential to truly heal tissue in pioneering ways, while having a favorable risk-benefit ratio, that makes it such a promising option.

A team of researchers from Harvard Medical School have found promising findings to help improve pain-related mood symptoms in patients that suffer from chronic lower back pain through the process of transcranial direct-current stimulation (tDCS).
Most therapies focus on managing the sensory component of pain. But most treatment options, such as nonsteroidal anti-inflammatory drugs, muscle relaxants, and opioids have serious side effects for both the short-term and the long term.
However, a non-invasive neuromodulation technique, tDCS may be used to alter neuronal activity in selected brain regions, such as the anterior cingulate cortex, which is a key region of the brain involved in the processing of pain.
In the study, twenty-one participants suffering from chronic lower back pain (LBP) for at least 6 months were assigned to the tDCS treatment, or a placebo group. The active treatment group received tDCS treatments targeting the dorsal anterior cingulate cortex (dACC) were administered once per day, 20 minutes per session, for 10 consecutive weekdays. The placebo group received a fake treatment, of briefly adjusting electric currents to reproduce the sensations associated with active tDCS.
By the end of the study, Patients reported significant improvement in pain across many different pain measurement scales. After six weeks, patients receiving the tDCS treatment continued to show significant improvement in LBP when assessed, compared to the in the placebo group.
tDCS is a promising form of therapy as it is fairly non-invasive, there are no risks of this therapy as there with the use of opioids, and it significantly lowers back pain, with long lasting effects.

Continuity of care is a long-standing feature of healthcare, especially of general practice. It is associated with increased patient satisfaction, increased take-up of health promotion, greater adherence to medical advice and decreased use of hospital services. More recently, a systematic review revealed that increased continuity of care by doctors is associated with lower mortality rates. Across cultural boundaries, patients appear to benefit from continuity of care with both generalist and specialist doctors.
Continuity of care is the repeated contact between and individual patient and a doctor. This repeated contact gives patients and doctors the opportunity for improved understanding of each other’s views and priorities.
There is a clear rationale for the effectiveness of continuity of care as doctors collect ‘accumulated knowledge’ about an individual patient which they then use in subsequent consultations to tailor advice.
Continuity of care in general practice is associated with greater patient satisfaction, improved health promotion, increased adherence to medication and reduced hospital use, Given all these separate benefits, the question arises whether these extend to mortality rates. Death is clearly the most important and serious of all outcomes.
In a substantial majority of studies, higher levels of continuity of care with doctors were associated with lower mortality rates.
When a patient has been coming to the same doctor for a long time, it creates a dynamic where the doctor can understand the patients needs and can prescribe and treat them based on a history of past experiences during their time together. This ultimately benefits the patient because they can receive personalized treatments that are more effective than generalized treatments.
Stem cells have the potential to develop into different types of cells, which make them a valuable tool in treating various injuries that require the regrowth of cartilage. The abilities of fat-derived stem cells allow for it to be a versatile treatment method, that is able to address many osteoperothic and arthritic problems, which are traditionally known to be long and tedious.
Fat-derived stem-cell injections appear to be longer-lasting and may require only one injection. It’s a great alternative for a knee or hip replacement, which is costly and requires a long recovery process.
Stanford has also started a study that focuses on fat-derived stem cells. The two-year, randomized, controlled study will include about 100 patients. The researchers are harvesting fat cells from the knee using a minimally invasive surgery before inserting them back into the knee. Results show that patients have reduced inflammation and report feeling better, and becoming active again in just two months.
Dr. Menkin, who has years of experience performing minimally invasive procedures, is using fat-derived stem cells to address knee/shoulder and hip osteoarthritis and injuries.

